No Scalpel Vasectomy: Global Adoption Trends
Vasectomy has been recognized for decades as one of the most effective and reliable methods of permanent contraception for men. However, it was the development of the no scalpel vasectomy (NSV) in the early 1980s by Dr. Li Shunqiang in China that revolutionized male sterilization practices around the world. This minimally invasive technique offered fewer complications, quicker recovery, and reduced fear among men who had previously been reluctant to undergo the procedure.
Over the past four decades, global adoption trends of no scalpel vasectomy have provided fascinating insights into cultural attitudes, healthcare priorities, and evolving family planning strategies. While uptake varies significantly across countries, the global landscape reflects a steady movement toward wider acceptance of NSV as a safe, accessible, and effective contraceptive option.
This article explores how no scalpel vasectomy is being adopted globally, analyzing regional trends, cultural influences, healthcare system factors, and future outlooks.
The Origins of No Scalpel Vasectomy
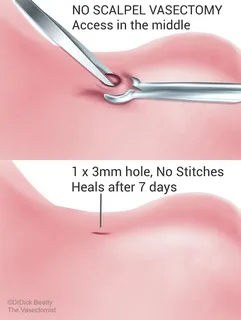
The no scalpel vasectomy was introduced in 1984 in China as a response to the need for a safer and more acceptable method of male sterilization. Traditional vasectomy, which required incisions and sutures, was often associated with pain, fear, and slower recovery. NSV solved these issues by using a sharp, pointed instrument to puncture the scrotal skin, allowing access to the vas deferens without large incisions.
The benefits quickly became clear:
- Reduced bleeding and infection risk
- No sutures required
- Shorter procedure time
- Faster return to normal activity
- High success rate with minimal complications
From China, NSV spread globally, supported by international health organizations, governments, and advocacy groups. Its spread, however, has been uneven across regions, shaped by social, cultural, and policy-related dynamics.
Global Adoption of No Scalpel Vasectomy
1. Asia
Asia is where NSV originated, and adoption trends vary by country.
- China:
In the 1980s and 1990s, NSV was aggressively promoted under the government’s family planning policies. Millions of procedures were performed, making China a global leader in NSV adoption. However, with the relaxation of the one-child policy, vasectomy rates—including NSV—have declined. - India:
India remains one of the largest adopters of NSV, largely due to government-sponsored family planning programs. Despite historical stigma associated with male sterilization, public health campaigns have increased awareness. NSV is particularly promoted in rural areas because of its simplicity and low complication rate. - Southeast Asia (Indonesia, Nepal, Thailand):
These countries have shown moderate uptake, often supported by international NGOs and local awareness initiatives. In Nepal, for example, “Vasectomy Camps” have been used to reach rural men, with NSV being the preferred method.
2. North America
- United States:
Vasectomy in general is relatively common, with NSV becoming the preferred method in clinical practice since the 1990s. Estimates suggest that about 500,000 vasectomies are performed annually in the U.S., with a majority now using the no scalpel approach. Adoption has been driven by patient demand for less invasive methods, as well as training programs for urologists. - Canada:
Canada has one of the highest vasectomy rates in the world, with about 20% of men opting for sterilization. NSV is the gold standard here, widely covered by healthcare systems and strongly supported by family planning providers.
3. Europe
In Europe, adoption varies by region.
- Western Europe (UK, Netherlands, Belgium):
NSV has been widely adopted, with vasectomy being a well-accepted contraceptive method. Public healthcare coverage and progressive cultural attitudes toward male participation in contraception drive these trends. - Southern Europe (Italy, Spain, Portugal):
Vasectomy rates, including NSV, remain low compared to other forms of contraception, largely due to cultural and religious attitudes that emphasize female-centered methods like the pill or IUDs. - Eastern Europe:
Adoption is very limited, with vasectomy still uncommon and often stigmatized. NSV is available but not widely practiced.
4. Latin America
Latin America has shown significant adoption of NSV in some countries, supported by family planning programs.
- Brazil:
Vasectomy, including NSV, has gained popularity since the 1990s as part of public healthcare initiatives. Public campaigns and free services have normalized male sterilization. - Mexico and Central America:
Government and NGO programs have promoted NSV in rural and underserved areas, though cultural resistance still exists in some communities.
5. Africa
Adoption of no scalpel vasectomy in Africa has been slow, but steady progress is being made.
- South Africa:
NSV is available in public hospitals and promoted as part of HIV prevention and family planning programs. Adoption is growing but still limited compared to female sterilization. - East Africa (Kenya, Uganda, Tanzania):
International NGOs and government programs have introduced NSV as part of family planning outreach. Uptake is gradually improving, especially in rural areas where long-term contraceptive options are limited. - West Africa:
Vasectomy in general remains rare, with strong cultural and religious barriers limiting acceptance.
6. Oceania
- Australia and New Zealand:
Both countries report high vasectomy rates, with NSV being the standard method. Adoption is supported by healthcare systems, strong family planning networks, and cultural openness toward male responsibility in contraception.
Cultural Influences on NSV Adoption
Cultural perceptions strongly shape global adoption patterns of no scalpel vasectomy.
- Gender roles: In societies where contraception is viewed as primarily a woman’s responsibility, male sterilization—including NSV—is less accepted.
- Religious beliefs: Strong opposition from religious institutions in some regions (particularly Catholic-majority countries) reduces adoption.
- Stigma and myths: Misconceptions about vasectomy causing impotence or reduced masculinity hinder uptake.
- Family planning policies: Countries with strong government involvement in reproductive health often have higher NSV adoption.
Healthcare System and Policy Impact
The structure of healthcare systems plays a central role in shaping NSV adoption:
- Public healthcare coverage: Countries like Canada and the UK have high adoption due to full or partial coverage of vasectomy.
- NGO involvement: In developing countries, international organizations (e.g., Marie Stopes International) provide NSV services in underserved areas.
- Physician training: Access to trained providers is a critical factor. Many regions still lack sufficient urologists or surgeons trained in NSV.
Future Trends in Global NSV Adoption
- Rising Male Participation in Contraception
As gender roles evolve, more men are expected to take responsibility for family planning. - Expansion of NGO Programs
International partnerships are likely to increase NSV access in Africa and South Asia. - Normalization Through Education
Public campaigns debunking myths about vasectomy will further reduce stigma. - Technological Advancements
Refinements in surgical instruments and techniques may make NSV even more efficient and accessible. - Shift Toward Minimally Invasive Care
As healthcare systems prioritize patient comfort and quick recovery, NSV will continue to be favored over traditional vasectomy.
Case Studies: Lessons from Global Adoption
- China: Demonstrated how strong government support can rapidly increase NSV adoption, though political and demographic shifts can also reverse the trend.
- Canada: Showed that universal healthcare and normalization of male sterilization create long-term, sustainable adoption.
- India: Proved that even in conservative societies, outreach and education can overcome stigma.
- Africa: Illustrates the need for persistent efforts to address cultural resistance and ensure trained providers.
Conclusion
The global adoption trends of no scalpel vasectomy reveal a complex interplay between culture, healthcare systems, policies, and patient perceptions. While some countries have embraced NSV as the gold standard for male sterilization, others still lag behind due to social stigma, limited access, and competing contraceptive priorities.
Nevertheless, the global direction is clear: no scalpel vasectomy is becoming increasingly recognized as a safe, effective, and male-friendly method of contraception. With ongoing education, healthcare support, and cultural shifts toward shared contraceptive responsibility, NSV is likely to see greater adoption worldwide in the coming decades.
FAQs
1. Why is no scalpel vasectomy more widely adopted in some countries than others?
Adoption depends on cultural attitudes, healthcare policies, and availability of trained providers. Countries with supportive healthcare systems and open attitudes toward male contraception report higher uptake.
2. Is no scalpel vasectomy popular in developing countries?
Yes, but adoption is uneven. While countries like India and Nepal have embraced NSV through outreach programs, other regions, especially in Africa, face cultural and logistical barriers.
3. Will the global adoption of no scalpel vasectomy continue to grow?
Yes. As stigma decreases, education improves, and more healthcare providers are trained, global adoption is expected to expand, particularly in regions currently underserved.